Magic Wand Combines Movement and Technology
(NewsUSA) - Technology is part of children’s lives, and although excessive screen time is a concern, other types of technology can be an enhancement to early childhood education.
- Technology is part of children’s lives, and although excessive screen time is a concern, other types of technology can be an enhancement to early childhood education.
The Kinoo Magic Wand is a screenless, smart device that young children can use independently or with family members. The 4-inch wand features three illuminated bulbs and a speaker to produce light, color and sound. Children use the wand to add an essential element of movement-based learning to games and activities in the Move & Master book (mBook), High Five magazine Kinoo Special Edition and more that are compatible with the wand.
The activities accompanying the wand were developed in partnership with Highlights for Children, the classic children’s publisher of magazines and books.
The wand acts as a tool to help engage children as they work through letters, phonics and reading, as well as body exercises, music instruments, Hidden Pictures and others. The activities are also designed to help build life skills such as creativity, collaboration, curiosity and critical thinking.
“Brain research has validated 'physical movement' as a powerful accelerant to learning and development for kids when coupled with visual and auditory learning modalities,” says Jim Marggraff, CEO and founder of Kinoo.
“While screen time has become a part of everyday parenting and education, it has reduced the time kids spend actively engaging and socializing. Kinoo was founded to combine leading edge technologies with developmental research to produce breakthroughs in learning for all children,” says Marggraff, who created the transformational, award-winning LeapPad Learning System.
To celebrate the launch of the Kinoo Magic Wand, in partnership with Highlights for Children, Kinoo is hosting the Kinoo Magic Wand Contest. The winning family receives a free trip to Los Angeles, Calif., and will star in Kinoo’s 2023 product commercial. Many families around the countries have participated in the #kinoomagicwand social campaign.
Parents can also use the Kinoo Magic app to customize their wands with ongoing new releases of content and activities from an expanding library. Another bonus: the Kinoo Connect app enables children to safely play collaborative, curated games while video chatting with selected individuals, such as a remote family member.
The Kinoo Magic Wand with High Five magazine Kinoo Special Edition by Highlights for Children is a perfect holiday gift.
Visit kinoo.com for more information.



 -
- 
 - The holiday season is coming, and with the return to in-person events, everyone wants to look their best. But many people who might consider a skin-tightening treatment shy away from needles, and have concerns about fillers and chemicals. Apex Center for Regenerative Medicine offers an alternative.
- The holiday season is coming, and with the return to in-person events, everyone wants to look their best. But many people who might consider a skin-tightening treatment shy away from needles, and have concerns about fillers and chemicals. Apex Center for Regenerative Medicine offers an alternative.  - “This is a work of fiction -- really.” It’s hard for poet Pasquale Trozzolo to convince us that his brilliant “UN/Reconciled:” (Kelsay Books) is not intended to portray any person, or combination of persons living or dead. Attribute that to the passion dripping from each vignette in this marvelous collection of 29 poems on a journey to the center of that most complex human experience: romantic love gone off.
- “This is a work of fiction -- really.” It’s hard for poet Pasquale Trozzolo to convince us that his brilliant “UN/Reconciled:” (Kelsay Books) is not intended to portray any person, or combination of persons living or dead. Attribute that to the passion dripping from each vignette in this marvelous collection of 29 poems on a journey to the center of that most complex human experience: romantic love gone off.  The collection reminds couples that relationships take work, even when in a powerful love. It is essential to capture the magnetic tension experienced in the first weeks and months of the relationship and find ways to keep discovering it, even as the mundane of ordinary life interferes.
The collection reminds couples that relationships take work, even when in a powerful love. It is essential to capture the magnetic tension experienced in the first weeks and months of the relationship and find ways to keep discovering it, even as the mundane of ordinary life interferes.  Writes Shawn Aveningo Sanders, author of “What She Was Wearing,” “Like a siren’s sultry song haunts the sailor, a mysterious woman floats in and out of the speaker’s life. Trozzolo takes us on a poetic journey through a salacious love affair that has such a hold on him that he still sees her everywhere … The poem vignettes deftly echo the brief, dangerous moments the two lovers shared.”
Writes Shawn Aveningo Sanders, author of “What She Was Wearing,” “Like a siren’s sultry song haunts the sailor, a mysterious woman floats in and out of the speaker’s life. Trozzolo takes us on a poetic journey through a salacious love affair that has such a hold on him that he still sees her everywhere … The poem vignettes deftly echo the brief, dangerous moments the two lovers shared.”  -
-  Dancing in the River”
Dancing in the River”  “Old Paradigms Die Hard”
“Old Paradigms Die Hard” “It's A Very If Not You Then Who? Christmas!”
“It's A Very If Not You Then Who? Christmas!” “Giggles Galore”
“Giggles Galore”
 - The holiday season is here, and people are eager for some well-earned self-indulgence.
- The holiday season is here, and people are eager for some well-earned self-indulgence.
 - This holiday season, the U.S. Marine Corps Reserve Toys for Tots Program celebrates its 75th year of delivering hope and joy to children in need across the Nation. Marines and volunteers are busy engaging with local businesses, media and community leaders to collect new, unwrapped toys to ensure that every child in need in their community has a present to open on Christmas morning.
- This holiday season, the U.S. Marine Corps Reserve Toys for Tots Program celebrates its 75th year of delivering hope and joy to children in need across the Nation. Marines and volunteers are busy engaging with local businesses, media and community leaders to collect new, unwrapped toys to ensure that every child in need in their community has a present to open on Christmas morning. 
 - Caribbean travel is back, and many favorite spots are expanding their offerings to meet a greater range of tastes and interests. If you or your travel companions are vegan, for example, you can find many more opportunities to relax and indulge.
- Caribbean travel is back, and many favorite spots are expanding their offerings to meet a greater range of tastes and interests. If you or your travel companions are vegan, for example, you can find many more opportunities to relax and indulge. 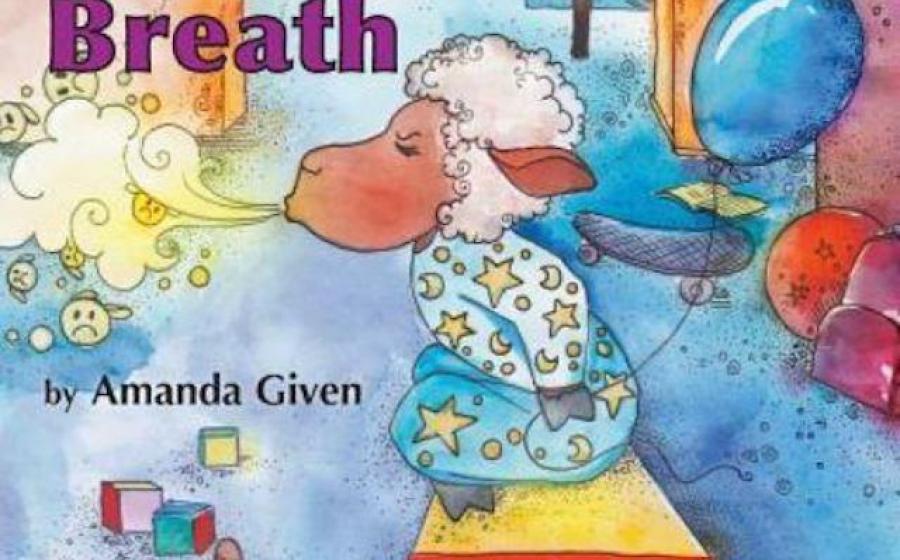
 - Amanda Given, an author, speech language pathologist, yogi, mother, mental health advocate and child at heart, has given us a charming story with colorful and playful illustrations that will help any child, young or old, open up and learn to deal with their feelings, all by learning about Balloon Breath.
- Amanda Given, an author, speech language pathologist, yogi, mother, mental health advocate and child at heart, has given us a charming story with colorful and playful illustrations that will help any child, young or old, open up and learn to deal with their feelings, all by learning about Balloon Breath.  “I wrote my book to help children and their caregivers manage their big emotions,” says the author, whose story is complemented with marvelous illustrations by Polina Hrytskova. The book also includes fun and easy activities for parents, adult guardians, teachers and children to reinforce the message.
“I wrote my book to help children and their caregivers manage their big emotions,” says the author, whose story is complemented with marvelous illustrations by Polina Hrytskova. The book also includes fun and easy activities for parents, adult guardians, teachers and children to reinforce the message. 
 - Put the fun in your fundraising efforts with the power of coffee, a user-friendly website and the business acumen of a veteran-led nonprofit company that has been building donor trust since 2016.
- Put the fun in your fundraising efforts with the power of coffee, a user-friendly website and the business acumen of a veteran-led nonprofit company that has been building donor trust since 2016. 

